Why Hyperbaric Treatment Saves Divers' Lives
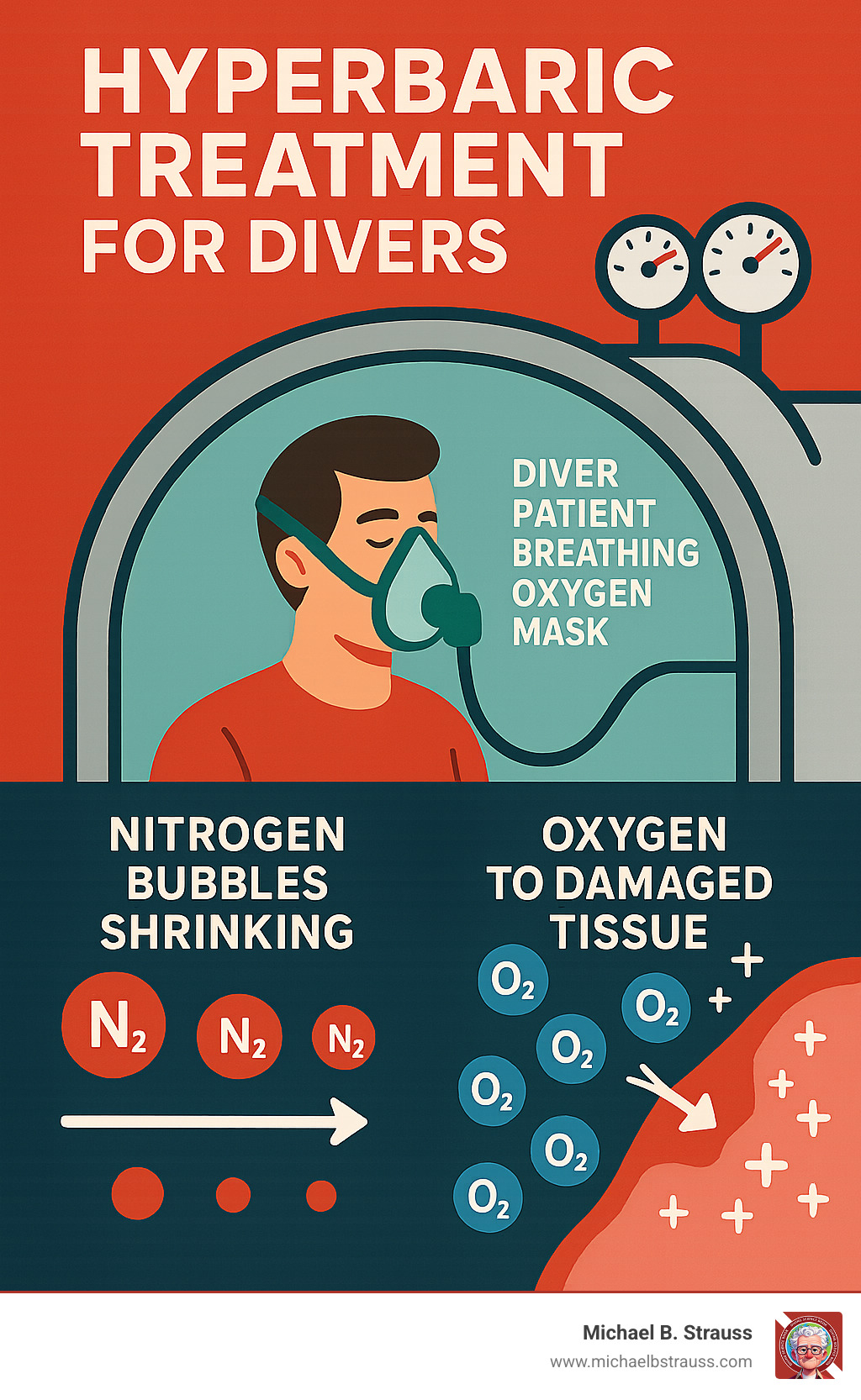
Hyperbaric treatment for divers is the definitive medical intervention for life-threatening diving injuries like decompression sickness (the bends) and arterial gas embolism. This therapy uses pressurized chambers and 100% oxygen to shrink dangerous gas bubbles in the bloodstream and deliver concentrated oxygen to damaged tissues.
When nitrogen bubbles form in a diver's tissues during a rapid ascent, hyperbaric oxygen therapy saves lives. The treatment follows established protocols, such as the U.S. Navy Treatment Table 6, which pressurizes patients to the equivalent of 60 feet underwater while they breathe pure oxygen. Treatment typically lasts between 1.5 to 5 hours, with a high success rate for patients who receive prompt care.
The science is straightforward but powerful. Higher pressure shrinks gas bubbles according to Boyle's Law, while concentrated oxygen accelerates healing and helps eliminate dangerous gases from the body. This dual action makes hyperbaric treatment the gold standard for diving emergencies, available 24/7 at specialized medical facilities worldwide.
Terms related to Hyperbaric treatment for divers:
The Core of Hyperbaric Treatment for Divers
When you're exploring the underwater world, you're entering an environment that can sometimes challenge your body in unexpected ways. That's where hyperbaric treatment for divers becomes absolutely essential - it's the medical lifeline that can literally save your life when diving goes wrong.
Let's explore the science behind this remarkable treatment and understand exactly how it helps divers recover from serious diving injuries.
Key Diving Conditions Treated with HBOT
The most common reason divers need hyperbaric treatment for divers is Decompression Sickness (DCS), also known as "the bends." During a dive, nitrogen from breathing air dissolves into body tissues. Ascending too quickly causes this nitrogen to form bubbles in blood and tissues, similar to opening a shaken soda bottle. These nitrogen bubbles can cause painful joint pain and serious neurological symptoms.
DCS can manifest as skin bends (itching and rashes) or severe spinal cord DCS, which may lead to paralysis. Another critical condition is Arterial Gas Embolism (AGE), where gas bubbles enter the arterial bloodstream, causing blocked blood flow to vital organs like the brain. AGE is often caused by holding one's breath during ascent.
Both DCS and AGE are forms of Decompression Illness (DCI), a medical emergency requiring immediate hyperbaric treatment for divers. Prompt treatment is crucial for a full recovery, making early symptom recognition vital for every diver.
For a deeper understanding of where and why decompression sickness occurs, check out More info about Decompression Sickness.
How HBOT Combats Diving Injuries
The science behind hyperbaric treatment for divers relies on fundamental laws of physics.
Boyle's Law states that as pressure increases, gas volume decreases. Inside a hyperbaric chamber, increased pressure shrinks the dangerous nitrogen bubbles in the body, reducing blocked blood flow and pressure on tissues.
Henry's Law explains that more gas dissolves in a liquid under higher pressure. Breathing pure oxygen in the chamber significantly increases the amount of oxygen dissolved in blood plasma. This hyperoxygenation has several benefits: it accelerates the removal of nitrogen, reduces tissue swelling, and helps prevent reperfusion injury (damage that occurs when blood flow returns to tissue).
This oxygen-rich environment also promotes new blood vessel growth and boosts the immune response, aiding long-term healing. By shrinking bubbles and flooding the body with healing oxygen, hyperbaric treatment for divers tackles the problem from multiple angles.
To learn more about the intricate science behind decompression, visit More info about the science of decompression.
Understanding Chamber Types for Hyperbaric Treatment
Hyperbaric treatment for divers occurs in a specialized pressure vessel called a hyperbaric chamber. There are two main types.

- Monoplace chambers treat one person at a time. The patient lies in an individual pod filled with pure oxygen, which they breathe directly.
- Multiplace chambers are larger, treating several patients simultaneously. These chambers are pressurized with air, and patients breathe pure oxygen through a mask or hood. Inside attendants (tenders) can provide care during treatment.
Both chamber types are equally effective for diving injuries. All medical chambers must meet strict ASME PVHO standards for safety, unlike unapproved "soft" chambers. Safety is critical in the oxygen-rich environment. Patients must remove fire risks like petroleum products, lighters, and battery-powered devices. You'll be given cotton clothing to wear, as synthetic materials can create static electricity. Medical staff will guide you through all safety protocols to ensure your treatment is both effective and safe.
Navigating Your Treatment: A Diver's Guide
Experiencing a diving-related injury can be unsettling, but knowing what to expect during and after hyperbaric oxygen therapy can help alleviate anxiety and empower us through the recovery process. This section provides practical information for divers who may need to undergo this vital treatment.
The Treatment Process: What to Expect
Knowing what to expect during hyperbaric treatment for divers can help alleviate anxiety. A healthcare team will guide you, but here is a general overview.
Preparation and Entry: Before treatment, you'll change into hospital-approved cotton clothing to minimize fire risk. All unapproved personal items, like electronics or petroleum-based products, must be removed. You will then lie down in a monoplace chamber or sit/lie in a multiplace chamber, with communication available via an intercom.
Pressurization and Equalization: As the chamber pressurizes, you'll feel fullness in your ears, similar to a diving descent. It is essential to equalize your ears by swallowing, yawning, or using the Valsalva maneuver. Staff will guide you on these techniques.
During Treatment: Protocols for diving injuries often follow the U.S. Navy Treatment Tables. A common regimen, Treatment Table 6 (USN TT6), involves pressurizing the chamber to 2.8 atmospheres absolute (ATA)—equivalent to 60 feet of seawater. You will breathe 100% oxygen through a mask or hood, with scheduled "air breaks" to prevent oxygen toxicity. A USN TT6 treatment lasts just under five hours, during which you can rest.

Decompression and Post-Treatment: After the treatment, the chamber is slowly decompressed. You may feel tired or lightheaded afterward, so arrange for someone to drive you home. Depending on the severity of the injury, multiple sessions may be required. The decision to use HBOT is made with a healthcare provider based on your specific condition.
For an in-depth look at various approved HBOT treatments, we can consult the resources provided by the Undersea and Hyperbaric Medical Society.
Risks, Side Effects, and Safety Protocols for Hyperbaric Treatment for Divers
While hyperbaric treatment for divers is generally safe, it's important to be aware of potential risks and side effects. Most are mild and temporary.
Common Side Effects: The most frequent issue is ear and sinus barotrauma due to pressure changes; proper equalization techniques are key to prevention. Other common effects include temporary vision changes (nearsightedness), fatigue, headaches, and claustrophobia. Informing staff about anxiety is important for receiving support.
Rare but Serious Complications: Though rare, oxygen toxicity can affect the central nervous system (seizures) or lungs. Carefully monitored protocols, including "air breaks," are designed to prevent this. The oxygen-rich environment also creates a fire risk, which is managed with strict protocols regarding clothing and personal items.
Safety Protocols and Regulations: Patient safety is paramount. Facilities operate under strict regulations. All chambers must meet ASME PVHO standards for design and safety. Accredited facilities employ highly trained staff and conduct thorough patient screenings to identify contraindications, such as an untreated pneumothorax. Understanding these robust safety measures allows patients to approach treatment with confidence.
For comprehensive safety guidelines, we can refer to the US Navy Diving Manual safety guidelines.
Emergency Planning and Accessing Hyperbaric Treatment for Divers
Preparedness is key to diving safety, including knowing how to access hyperbaric treatment for divers in an emergency. Immediate treatment for decompression accidents can be life-saving.
Immediate Actions and Emergency Contact: If Decompression Illness (DCI) is suspected, first aid is critical. Administer 100% oxygen, contact emergency medical services (EMS), and call the Divers Alert Network (DAN) Emergency Hotline (+1-919-684-9111), which is available 24/7. DAN provides expert guidance and helps coordinate care with available hyperbaric facilities. Do not show up at a facility unannounced; coordination through EMS and DAN is essential.
Availability and Accessibility Challenges: Accessing a hyperbaric chamber for an acute dive injury can be challenging. Many hospitals now focus on elective treatments, reducing 24/7 emergency availability. Diving in remote locations further complicates access. Transporting an injured diver also requires care; aircraft must maintain a cabin pressure at or near sea level (1 ATA) to avoid worsening the condition.
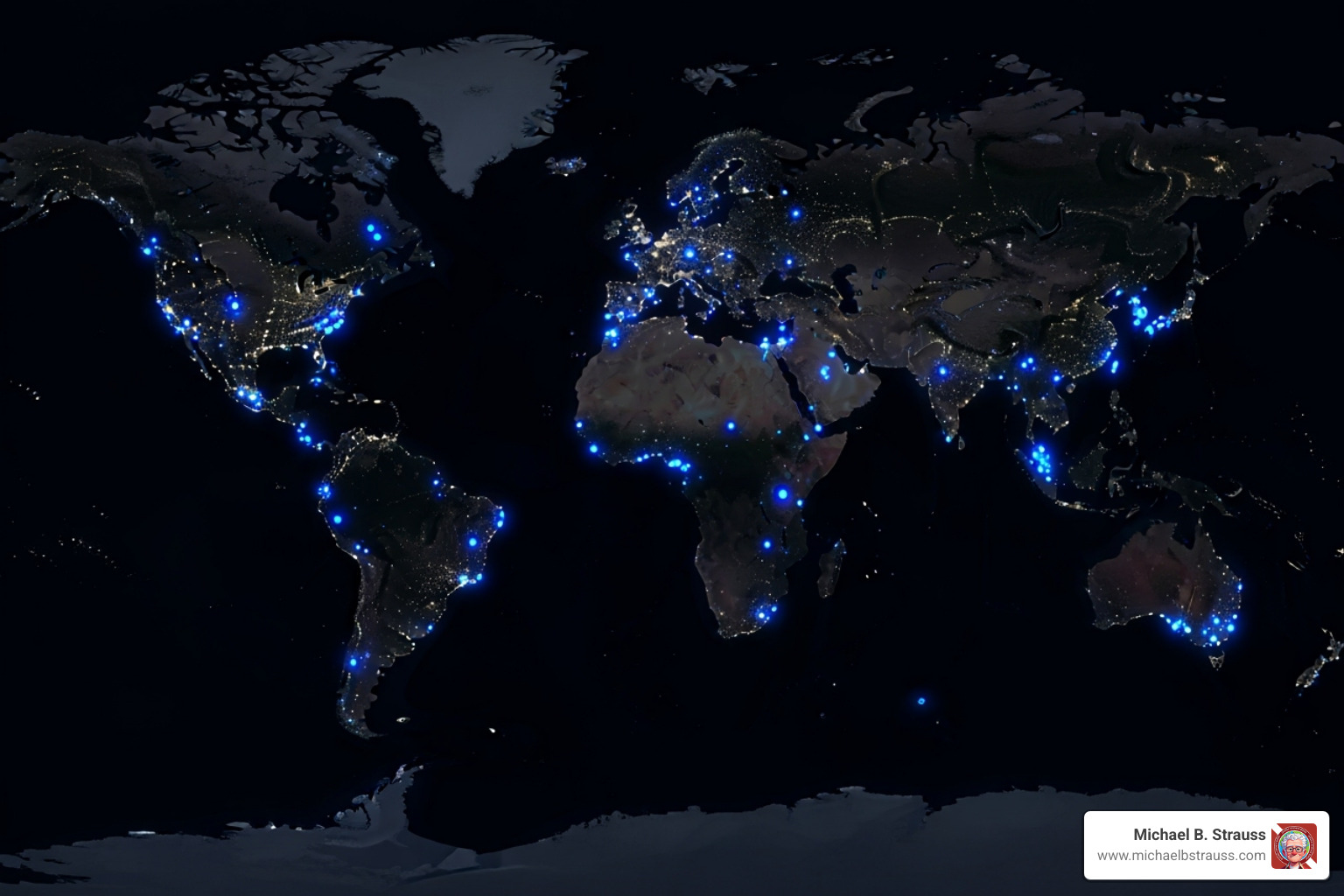
Emergency Action Plan (EAP): Every diver should have an EAP for each dive, including the location of the nearest hyperbaric facility, emergency contacts (EMS, DAN), and knowledge of DCI first aid.
Prioritizing safety ensures every dive is enjoyable. Dr. Michael B. Strauss, a renowned expert in diving safety, offers invaluable insights in his comprehensive diving books. These books are essential reads for both new and experienced divers, providing guidance on safety, emergency preparedness, and diving medicine. By staying informed and prepared, we can enjoy the underwater world responsibly.
To learn more, get your copy of Diving Science Revisited today.
DISCLAIMER: Articles are for "EDUCATIONAL PURPOSES ONLY", not to be considered advice or recommendations.






