Why Hyperbaric Treatment for Divers Saves Lives
Hyperbaric treatment for divers is the definitive medical intervention for decompression sickness (DCS) and arterial gas embolism (AGE), the most serious diving-related injuries. These conditions occur when nitrogen bubbles form in the blood and tissues after a diver surfaces too quickly, leading to symptoms from joint pain to paralysis or death.
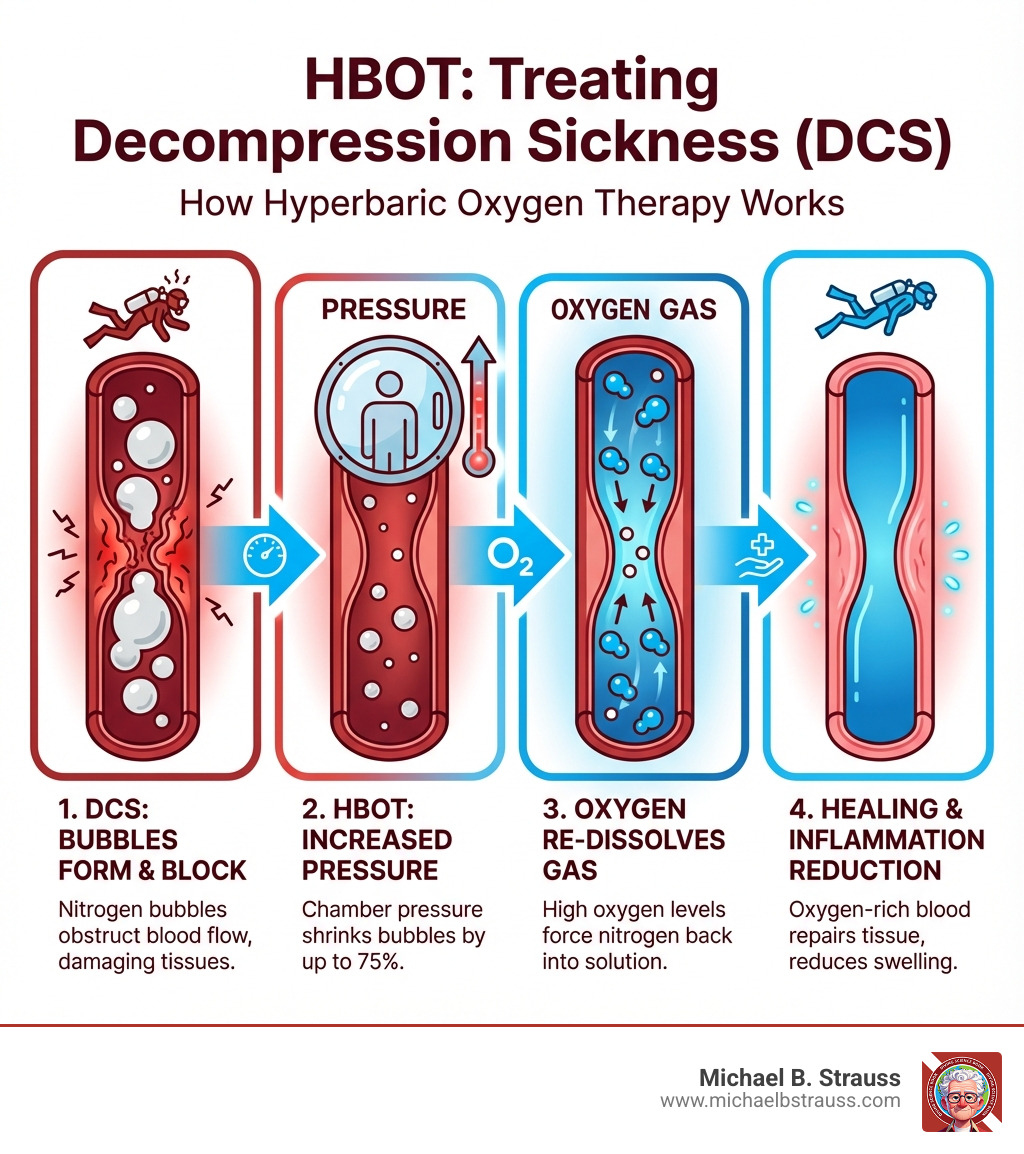
Hyperbaric oxygen therapy (HBOT) reverses this dangerous state. By placing a diver in a chamber pressurized to 2-3 times normal atmospheric pressure and having them breathe 100% oxygen, the treatment shrinks dangerous gas bubbles, forces nitrogen back into solution, and floods the body with oxygen to heal damaged tissues. These principles are based on U.S. Navy treatment protocols that remain the worldwide gold standard.
The immediate availability of hyperbaric treatment can mean the difference between life and death for an injured diver. However, a growing crisis threatens diver safety as the number of hyperbaric chambers providing 24/7 emergency services shrinks, driven by hospital business models favoring outpatient care. Understanding how HBOT works and where to access it is essential knowledge for every diver.
Important hyperbaric treatment for divers terms:
The Science and Application of Hyperbaric Treatment for Divers
How HBOT Treats Decompression Sickness (DCS) and Gas Embolism (AGE)
At its core, hyperbaric treatment for divers applies fundamental gas laws to reverse diving injuries.
- Boyle's Law explains that gas volume is inversely proportional to pressure. By increasing pressure inside a hyperbaric chamber, the dangerous nitrogen bubbles causing DCS and AGE are physically compressed, reducing their size and relieving blockages in blood vessels.
- Henry's Law states that more gas dissolves into a liquid under higher pressure. HBOT uses this principle by increasing the pressure of 100% oxygen, which helps re-dissolve the harmful nitrogen bubbles back into the bloodstream so they can be safely eliminated from the body.
Beyond addressing the bubbles directly, HBOT provides other critical healing benefits. Breathing pure oxygen under pressure causes hyperoxygenation, dramatically increasing the oxygen carried by blood plasma. This allows oxygen to reach tissues deprived of blood flow, which is vital for cellular repair. The therapy also reduces inflammation, prevents secondary damage known as reperfusion injury, and stimulates the growth of new blood vessels to aid in long-term recovery.
For a deeper dive into the physics of decompression, explore More info about Decompression Science. You can also find extensive Scientific research on HBOT mechanisms detailing these benefits.
Types of Hyperbaric Chambers and Their Use for Divers
Not all chambers are the same, but many can effectively provide hyperbaric treatment for divers.
- Class A (Multiplace) Chambers: Large, room-like chambers that hold multiple patients and medical staff. They are pressurized with air, and patients breathe oxygen via masks or hoods.
- Class B (Monoplace) Chambers: Designed for a single patient, these clear tubes are pressurized entirely with 100% oxygen.
For treating Decompression Illness (DCI), both Class A and B chambers are equally effective when operated by trained staff in a healthcare setting. In remote locations, smaller transportable chambers can be vital for emergency treatment and transport.

A patient comfortably resting inside a monoplace hyperbaric chamber.
A Crucial Warning on Soft-Sided Chambers: Be wary of "mild" or "soft" inflatable chambers marketed for home or spa use. The FDA has only approved these for acute mountain sickness and they are not suitable for treating DCS or AGE. They often fail to meet critical safety standards for pressure vessels (ASME PVHO-1) and have been linked to tragic accidents. For more information, see the FDA Consumer Alert on soft-sided chambers.

Inside a multiplace hyperbaric chamber, allowing several patients to be treated simultaneously.
What to Expect During Your Hyperbaric Treatment for Divers
Knowing what to expect during hyperbaric treatment for divers can ease any anxiety. After changing into a hospital gown and removing prohibited items (like electronics and flammables), you will enter the chamber. The process involves three phases:
- Pressurization: The chamber is slowly pressurized. You will need to equalize the pressure in your ears by swallowing or yawning, just as you do when diving.
- Treatment: At the target pressure, you will breathe 100% oxygen through a mask or hood. The session will include scheduled "air breaks" (breathing normal air) to minimize the risk of oxygen toxicity.
- Decompression: The chamber is slowly returned to normal atmospheric pressure.
A standard treatment for DCS, like the U.S. Navy Treatment Table 6, lasts just under five hours, though other sessions can range from 90 minutes to several hours.
While generally safe, potential side effects include:
- Middle Ear Barotrauma: The most common side effect is ear pain from pressure changes.
- Sinus Pressure: Similar discomfort can occur in the sinuses.
- Fatigue: It's common to feel tired after a session.
- Oxygen Toxicity: A rare but serious risk managed with air breaks and careful monitoring.
A thorough medical evaluation is required before treatment. An untreated pneumothorax (collapsed lung) is the only absolute contraindication for HBOT. You should also inform the medical team about any colds, congestion, lung conditions, recent ear surgery, or claustrophobia, as these may require special consideration.
Access, Safety, and Broader Diving Considerations
The journey of hyperbaric treatment for divers extends beyond the chamber itself, encompassing vital considerations about access, safety standards, and alternative approaches in diverse environments.
The Current Landscape of Chamber Access and Safety Standards
Finding hyperbaric treatment for divers is becoming more difficult. Many hospitals are shifting their focus from 24/7 emergency dive injury services to more profitable outpatient wound care. This "chamber access crisis" means fewer facilities are available to treat acute DCS or AGE, making it harder to find timely care.
A visual representation of the shrinking access to 24/7 hyperbaric facilities for divers.
To ensure patient safety, reputable facilities are accredited by organizations like the Undersea and Hyperbaric Medical Society (UHMS) and adhere to strict safety codes like NFPA 99 (fire safety) and ASME PVHO-1 (pressure vessel construction). In an emergency, specialized 24-hour diving emergency hotlines are a crucial resource to help divers locate available and appropriate hyperbaric chambers.
In-Water Recompression and Other Hyperbaric Environments
While a certified chamber is the definitive treatment, other strategies exist for extreme circumstances.
In-Water Recompression (IWR) is a high-risk, last-resort procedure used in remote locations when a chamber is inaccessible. It involves returning a stable, conscious diver underwater to breathe pure oxygen at a shallow depth. However, IWR carries significant dangers, including drowning, oxygen toxicity, and environmental hazards. It should only be considered by highly trained teams with proper support and equipment.
Divers may also encounter other hyperbaric environments, such as saturation diving systems where commercial divers live under pressure for extended periods, or diving bells used for transport to deep work sites. Understanding the principles of pressure is key to safety in all these settings, a topic covered in-depth in More info about Diving Science.
Your Next Steps for Safe Diving and Emergency Preparedness
Education and preparedness are your best allies for safe diving. While hyperbaric treatment for divers is the definitive care for DCI, it is part of a broader emergency response.
The immediate response to a suspected dive injury should always be:
- Recognize the symptoms of DCS or AGE.
- Administer 100% surface oxygen immediately. This is the most critical first aid step.
- Seek a medical evaluation, even if symptoms improve.
Every diver should create a Dive Emergency Action Plan (EAP) that includes emergency contacts (such as a diving emergency hotline), the location of the nearest medical facility and hyperbaric chamber, and the diver's medical information.
Since few healthcare professionals specialize in dive medicine, it is vital for divers to be well-informed. Dr. Michael B. Strauss, a renowned expert in diving safety, offers invaluable insights in his comprehensive diving books. These resources are essential for understanding diving physiology, preventing injuries, and knowing how to respond in an emergency. By preparing for the worst, we can safely enjoy the best the underwater world has to offer.
To get or buy the book, please visit this link: Diving Science Revisited
DISCLAIMER: Articles are for "EDUCATIONAL PURPOSES ONLY", not to be considered advice or recommendations.






