When Joint Pain After Diving Signals Something Serious
Joint pain after diving can range from harmless muscle soreness to a life-threatening emergency called decompression sickness. Here's what we need to know:
Immediate Red Flags:
- Constant, deep aching pain in shoulders, elbows, or knees that doesn't improve with rest
- Pain that occurs within 1-24 hours after surfacing
- Joint pain combined with numbness, tingling, dizziness, or skin rash
- Pain unrelated to movement - stays the same whether you move or stay still
When It's Likely Just Muscle Soreness:
- Pain improves with rest and stretching
- Occurs in muscles you used heavily during the dive
- Responds to typical pain relievers
- No other concerning symptoms
Most recreational divers experience normal muscle fatigue after a dive. But joint pain after diving that feels different from typical soreness could be your body's warning sign of decompression sickness - also known as "the bends."
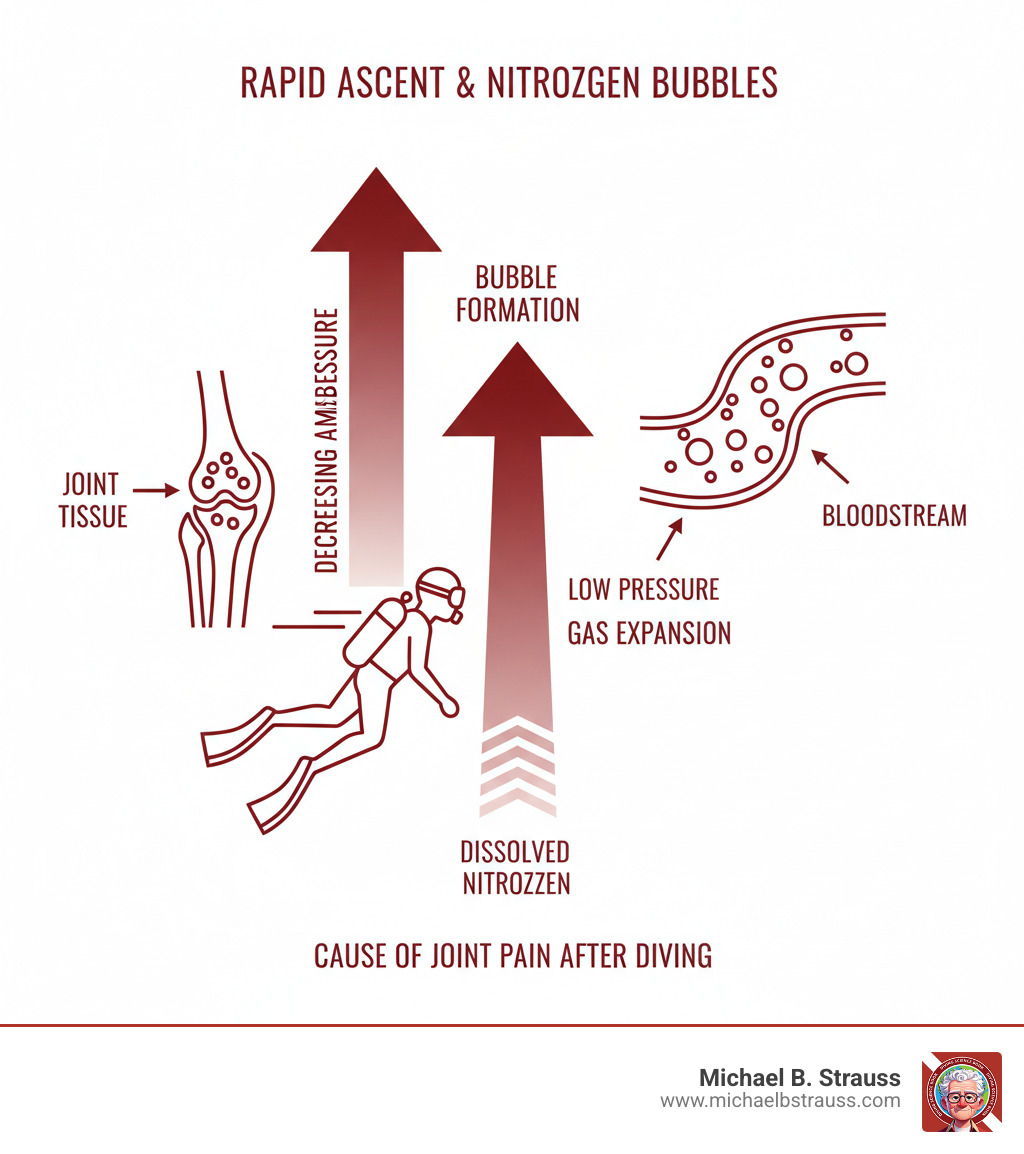
The condition occurs when nitrogen dissolved in your blood and tissues forms bubbles during ascent, similar to opening a carbonated drink. These bubbles can cause inflammation, block blood vessels, and damage tissue, leading to a characteristic deep, boring pain. Early recognition is critical, as the window for effective treatment is narrow and symptoms can rapidly progress.
Understanding Decompression Sickness and Joint Pain After Diving
As you descend, increasing water pressure forces nitrogen from your breathing gas to dissolve into your blood and tissues. This process follows Henry's Law, which states that the amount of gas dissolved in a liquid increases with pressure. While your body handles this during the dive, problems can arise during your ascent.
The Science Behind "The Bends": How Nitrogen Bubbles Cause Pain
Decompression sickness (DCS), or "the bends," occurs when dissolved nitrogen forms bubbles during ascent if you surface too quickly—similar to opening a shaken soda bottle. These bubbles can damage tissues, block blood vessels, and trigger an inflammatory response that produces pain-causing substances. This is why joint pain after diving is the most common DCS symptom; bubbles often form in and around joints, creating a deep, boring ache. By blocking blood flow, these bubbles starve tissues of oxygen and cause swelling and intense pain.
For a deeper understanding of how and where DCS develops, you'll find valuable insights in resources like Why and at What Sites Decompression Sickness Can Occur and Scientific research on Decompression illness.
Is It DCS? Recognizing the Telltale Symptoms
Recognizing DCS symptoms quickly can be life-saving. Joint pain after diving typically appears within the first hour after surfacing for about half of all cases, and within six hours for 90% of divers who develop the condition. However, symptoms can sometimes appear as late as 24 to 48 hours after your dive.
Medical professionals classify DCS into two main types:
Type I DCS is the milder form, affecting joints, skin, and lymphatics. The hallmark joint pain after diving strikes large joints like the shoulders and elbows. The pain is constant, deep, and "boring," and doesn't change with movement. You might also see skin symptoms like a mottled rash ("skin bend") or itching, which can sometimes signal more serious issues.
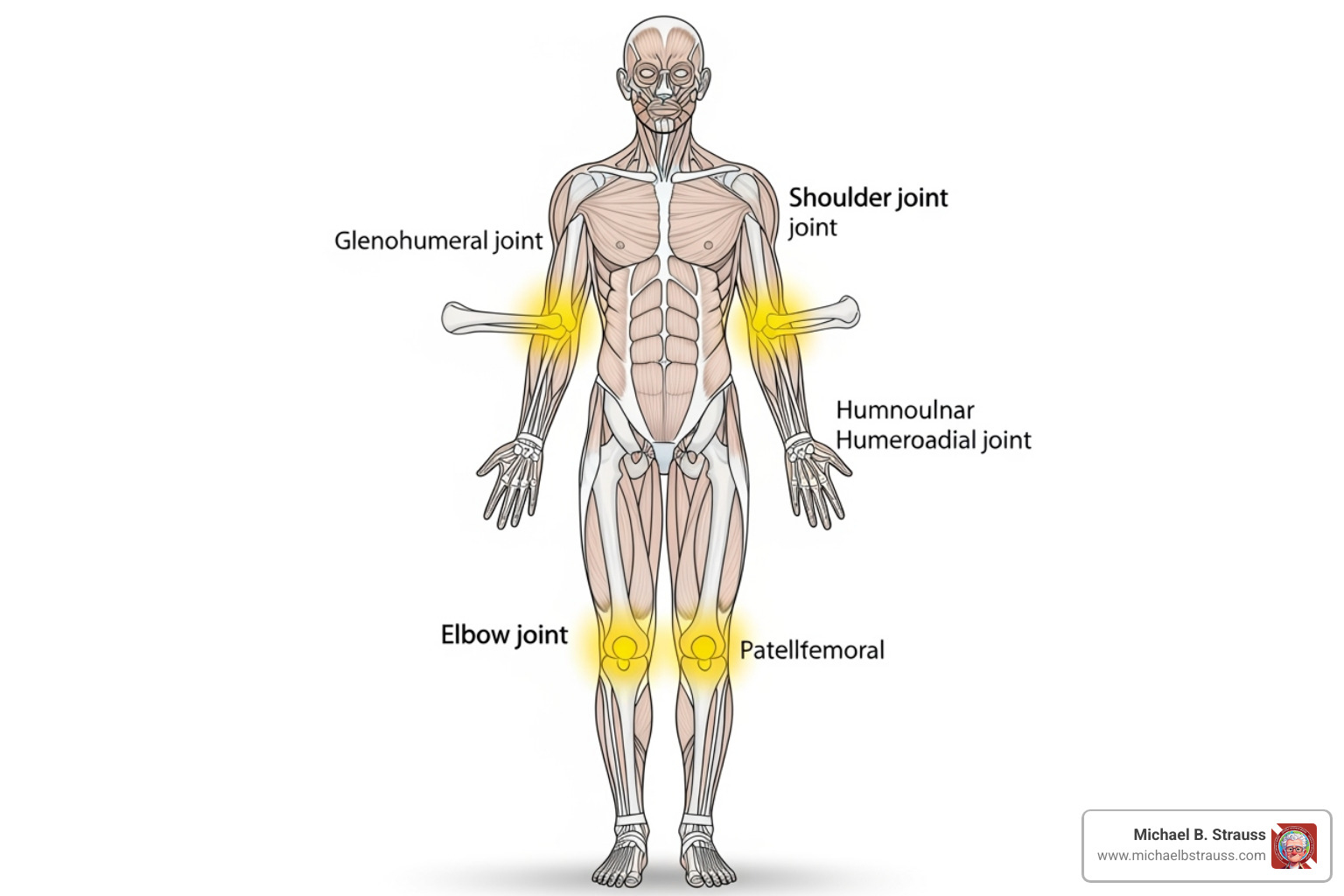
Type II DCS is more serious, affecting the brain, spinal cord, and respiratory systems. While joint pain after diving may be present, look for neurological red flags: numbness and tingling, weakness, dizziness, headaches, confusion, extreme fatigue, and balance problems. Severe cases can lead to paralysis or loss of consciousness. Respiratory symptoms like shortness of breath and chest pain ("the chokes") are a medical emergency.
The prevalence of joint pain after diving in DCS cases makes it a crucial diagnostic clue, but always stay alert for any accompanying neurological symptoms. For comprehensive information, consider exploring Evaluation and Management of Pain-Related Medical Problems of Diving.
Risk Factors and Distinguishing DCS from Other Dive-Related Pains
Not every ache after a dive signals decompression sickness. Understanding what increases your risk and how to distinguish DCS from normal post-dive soreness is key.
Several factors increase your risk of DCS and experiencing joint pain after diving:
- Dive Profile: Deep, long, or repetitive dives increase nitrogen absorption.
- Rapid Ascents: Ascending too quickly is a primary preventable risk factor.
- Physiological Factors: Dehydration, cold water, obesity, age, and heavy exertion can all impair nitrogen off-gassing.
- Medical Conditions: Heart conditions like a Patent Foramen Ovale (PFO), asthma, or other lung diseases significantly increase risk.
- Post-Dive Activities: Flying or traveling to a higher altitude too soon after diving can trigger DCS.
| Symptom Feature | DCS Joint Pain | Simple Muscle Strain | Compression Arthralgia |
|---|---|---|---|
| Pain Quality | Deep, boring, constant | Aching, improves with rest | Sharp, pressure-related |
| Response to Movement | No change with movement | Often improves with gentle movement | Worsens with pressure changes |
| Timing | Within 24 hours of surfacing | During or immediately after exertion | During descent or ascent |
| Location | Large joints (shoulders, elbows, knees) | Muscles used during dive | Joints experiencing pressure |
| Additional Symptoms | May include neurological signs | None beyond muscle soreness | Resolves quickly after dive |
Compression arthralgia is often confused with DCS. This condition causes joint pain during descent but typically resolves quickly after the dive, unlike DCS-related joint pain after diving.
When in doubt, always err on the side of caution. The window for effective DCS treatment is narrow, and early intervention can prevent long-term complications.
Your Action Plan: Prevention, Treatment, and Recovery
When it comes to joint pain after diving and decompression sickness, prevention is always the best strategy. Let's walk through what you need to know to stay safe and what to do if something goes wrong.
Proactive Prevention: Key Strategies to Avoid the Bends
Most cases of DCS-related joint pain after diving are preventable by respecting diving physics and allowing your body to safely off-gas nitrogen.
- Control Your Ascent: A slow, controlled ascent is critical. Follow your dive computer's ascent rate warnings. The U.S. Navy Diving Manual provides gold-standard decompression procedures.
- Make Safety Stops: Always perform a three to five-minute safety stop at around 15 feet, even on no-decompression dives. This gives nitrogen more time to safely leave your tissues.
- Plan Carefully: Use a modern dive computer and stay well within no-decompression limits, especially on repetitive dives. For a deeper understanding, Decompression Science offers valuable insights.
- Stay Hydrated, Avoid Alcohol: Proper hydration improves circulation and nitrogen elimination. Avoid alcohol before and after diving.
- Manage Post-Dive Activities: Avoid hot tubs or saunas immediately after diving, as rapid heating can promote bubble formation. Wait 12-24 hours before flying or traveling to altitude.
- Know Your Limitations: Be aware of how personal health factors, such as a Patent Foramen Ovale (PFO) or asthma, affect your risk. Always seek medical clearance if you have pre-existing conditions.

Treatment Protocols for DCS-Related Joint Pain After Diving
If you suspect DCS is causing your joint pain after diving, time is critical.
- Administer 100% Oxygen: This is the essential first aid for suspected DCS. High-flow oxygen helps wash nitrogen from your system and should be continued until you receive professional medical care.
- Seek Recompression Therapy: The definitive treatment for DCS is recompression in a hyperbaric oxygen chamber. This process re-pressurizes the body to shrink nitrogen bubbles, then gradually reduces pressure while you breathe pure oxygen, allowing for safe off-gassing.
Early treatment is key. Most divers respond well to a single hyperbaric session, with joint pain after diving often resolving quickly. Delays can reduce treatment effectiveness and, in rare untreated cases, lead to serious long-term problems like dysbaric osteonecrosis (bone tissue death).
After treatment, expect a waiting period of at least two weeks before diving again for mild cases, with longer recovery for severe episodes. The Undersea & Hyperbaric Medical Society provides excellent treatment and recovery guidelines. You might also find the research on Mammalian Divers fascinating.

When to Call a Professional for Joint Pain After Diving
The golden rule is: "When in doubt, check it out." It's always better to be safe than to risk permanent damage from untreated DCS.
Take your pain seriously. If joint pain after diving feels deep, constant, and doesn't improve with rest—especially in large joints within 24 hours of surfacing—seek help.
Watch for these red flags that require immediate medical attention:
- Neurological Symptoms: Any joint pain combined with numbness, tingling, weakness, dizziness, or skin changes.
- Respiratory Symptoms: Shortness of breath, chest pain, or coughing are medical emergencies.
Contacting a diving emergency hotline is crucial. These services can connect you with diving medicine experts for immediate guidance and help arrange transport to the nearest recompression facility.
Do not delay seeking treatment. Hyperbaric therapy is most effective within the first few hours. If air transport is required, the aircraft must be pressurized to sea level or fly at a very low altitude with continuous oxygen.
Diving medicine specialists like Dr. Michael B. Strauss have dedicated their careers to keeping divers safe. His comprehensive resources on diving science emphasize that education and preparedness are your best tools for handling any emergency. With proper knowledge and respect for the risks, you can explore the underwater world safely for years to come.

To learn more, get your copy of Diving Science, Revisited.
DISCLAIMER: Articles are for "EDUCATIONAL PURPOSES ONLY", not to be considered advice or recommendations.






