Understanding the Science Behind Neck Pain Relief
Manual cervical decompression science explains how controlled pulling forces on the neck can relieve pressure on spinal discs and nerves. By creating space between vertebrae, this technique reduces pain and restores function without surgery. The science centers on controlled force application to address the root cause of cervical pain.
Key Scientific Principles:
- Negative Pressure Effect: Gentle traction creates a vacuum inside spinal discs, helping pull herniated material back into place.
- Nerve Decompression: Widening the space between vertebrae releases pinched nerve roots.
- Improved Healing: Increased nutrient flow to damaged disc tissue supports natural repair.
- Pain Gate Closure: Mechanical stimulation can block pain signals from reaching the brain.
Understanding these biomechanics helps medical professionals determine when hands-on techniques are preferable to surgery or mechanical devices. This guide breaks down the research and clinical evidence supporting manual cervical decompression as an effective conservative treatment.

Easy manual cervical decompression science word list:
The Core Manual Cervical Decompression Science
Manual cervical decompression science involves a sophisticated interplay of biomechanics, physiology, and neurology. The goal is simple: create more space in your cervical spine to allow discs to heal and relieve pressure on nerves.
How It Works: Biomechanical and Neurological Principles
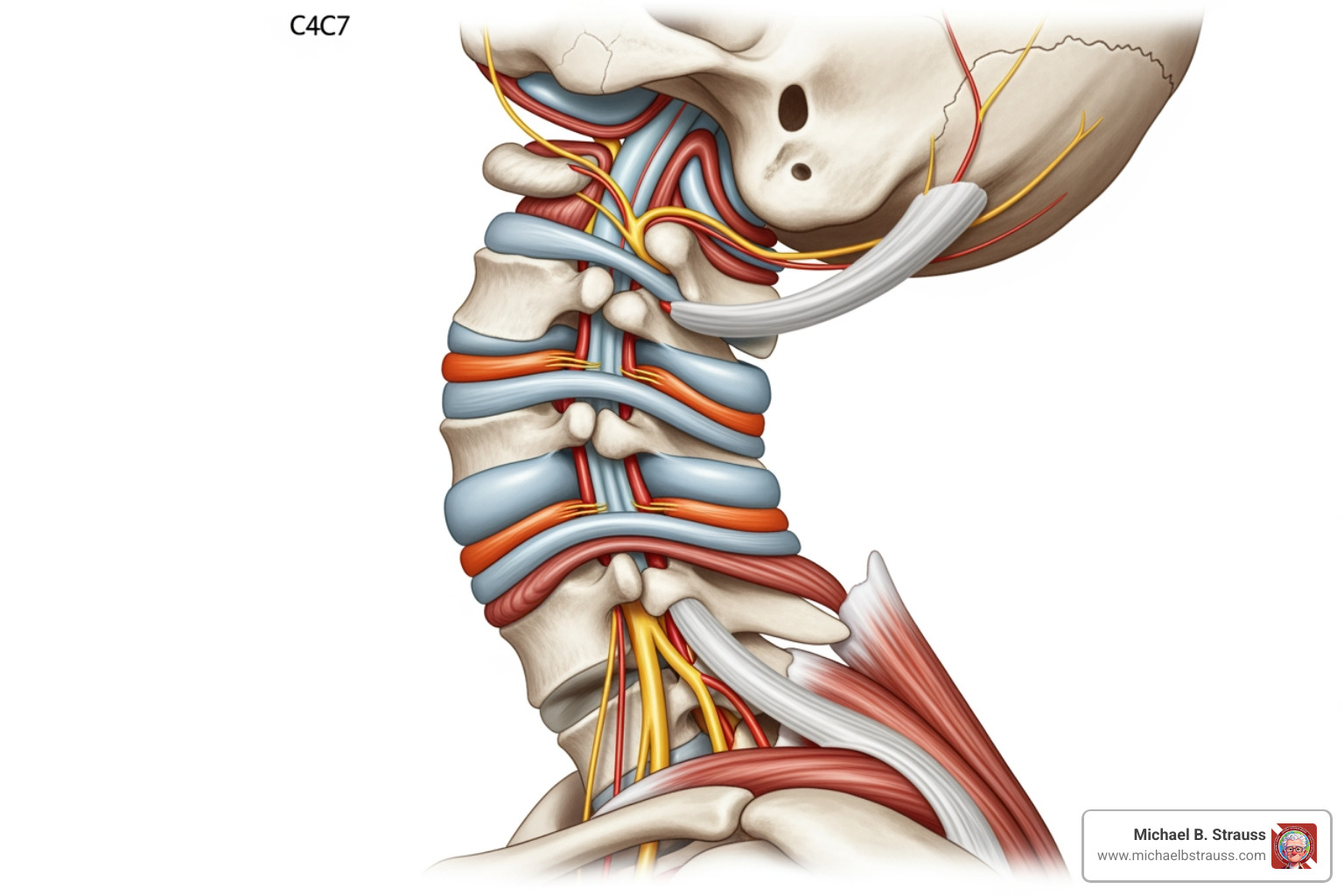
When intervertebral discs are compressed from injury or degeneration, they can bulge and press on nerve roots, causing pain, numbness, or weakness. Manual decompression aims to reverse this through several biomechanical responses.
A primary mechanism is creating negative intradiscal pressure. When a practitioner applies gentle, sustained traction, the vertebrae separate slightly. This creates a vacuum effect inside the disc, which can help pull bulging material back toward the center and away from nerve roots.
This process also improves nutrient diffusion. Adult spinal discs lack their own blood supply and depend on fluid movement from surrounding tissues for nutrients. Decompression acts like a pump, bringing in fresh nutrients and flushing out metabolic waste to support healing.
Additionally, the technique achieves foraminal widening. Spinal nerves pass through small openings between vertebrae (intervertebral foramina). When these openings narrow, nerves get pinched. Manual traction gently increases this space, decompressing the nerve roots.
Finally, decompression promotes soft tissue elongation, stretching tight muscles and ligaments to reduce spasms and improve flexibility. This mechanical stimulation also relates to the gate control theory of pain, where non-painful sensations from the stretching can block pain signals from reaching the brain, offering immediate relief. For more detail, scientific research on cervical traction mechanisms offers comprehensive insights.
Manual vs. Mechanical Traction: A Key Distinction
Understanding the difference between manual and mechanical cervical decompression is key. While both aim to relieve pressure, their methods differ significantly.
Manual cervical decompression involves a trained practitioner using their hands to apply traction. This allows for real-time adjustments based on the body's response, as the practitioner can feel muscle tension and joint resistance. This feedback loop improves safety and effectiveness, and provides diagnostic insights that inform the overall treatment plan.
Mechanical devices use harnesses, pulleys, or motorized units to apply a pre-set static (constant) or intermittent (on-off) force. While consistent, they lack the adaptive quality of human touch. Over-the-door traction is the simplest mechanical option for home use but offers the least control.
Here's how these approaches compare:
| Feature | Manual Cervical Traction | Mechanical Cervical Traction | Over-the-Door Cervical Traction |
|---|---|---|---|
| Application Method | Hands-on by a skilled practitioner | Device-driven (motorized, pulley systems) | Simple pulley system using a doorframe |
| Force Control | Highly variable, precise, real-time adjustment | Consistent, pre-set, can be static or intermittent | Often static, less precise control, dependent on weights |
| Patient Feedback | Direct, immediate, highly responsive | Indirect, patient communicates discomfort to operator | Limited, patient self-monitors |
| Adaptability | Excellent, can adjust angle, duration, and force instantly | Limited to device programming, less responsive to changes | Very limited, fixed angle and force |
| Diagnostic Value | High, practitioner can feel tissue response and joint play | Low, primarily therapeutic | None, solely therapeutic |
| Supervision Level | Constant, direct by practitioner | Can be supervised by a therapist, or self-administered (home units) | Self-administered, minimal supervision |
| Comfort & Safety | Generally high due to practitioner control | Varies, can be uncomfortable if not properly set | Can be uncomfortable, higher risk of improper use |
While mechanical traction has its place, the nuanced control of manual decompression often makes it preferable for acute or complex conditions.
The Practice of Manual Cervical Decompression Science
Performing manual cervical decompression requires anatomical knowledge and precise force application.
The patient is typically positioned supine (on their back) to keep the cervical spine neutral and encourage muscle relaxation. A relaxed state is essential for the treatment's effectiveness.
Practitioner hand placement is chosen based on the patient's condition. Common techniques include an occipital grip, cradling the back of the head, or a mastoid grip, with fingers placed behind the ears. The hold is secure but gentle to allow for controlled traction.
The axial traction force is applied along the spine's long axis, gently pulling the head away from the shoulders. The practitioner adjusts the angle of pull to target specific cervical segments. A smooth, steady pull is generated using body weight and leverage, not just arm strength.
Both sustained traction (a continuous pull) and intermittent traction (cycles of pull and release) are used. Sustained traction allows for a gradual stretch, while intermittent traction can be effective for promoting fluid exchange in the discs.
Throughout the process, the practitioner may perform soft tissue mobilization, gently massaging neck muscles to release tension. This combined approach addresses both spinal structures and surrounding soft tissues for more comprehensive relief.
Clinical Applications, Efficacy, and Safety
The science of manual cervical decompression science translates into a targeted, non-invasive approach for several debilitating cervical spine conditions, often providing relief where other treatments have failed.
Conditions Treated and Proven Benefits
Manual cervical decompression is effective for several common problems.
- Cervical Radiculopathy: This involves shooting pain, numbness, or tingling down the arm from a compressed nerve root. By creating space around the nerve, decompression can bring significant relief.
- Disc Herniation: When the soft center of a disc pushes out and presses on a nerve, decompression's negative pressure effect can help draw the material back, relieving the pressure.
- Cervical Spondylosis & Foraminal Stenosis: Age-related wear and tear can lead to bone spurs and disc degeneration, narrowing the nerve pathways (foraminal stenosis). Decompression gently widens these spaces.
- Muscle Spasms: The gentle stretching involved can break the pain-spasm cycle, allowing chronically tight neck muscles to relax.
The primary benefits include pain reduction, improved range of motion, and restored nerve function (less numbness/tingling, improved strength). Studies show significant pain relief, with many patients regaining the ability to perform daily activities without pain.
Evaluating the Evidence and Long-Term Outcomes
The practice of manual cervical decompression science is supported by a growing body of research, including systematic reviews and randomized controlled trials.
Evidence shows that decompression is most effective as part of a multimodal treatment approach. It is often integrated with chiropractic care to address joint dysfunction, physical therapy protocols for strengthening, and ergonomic advice to prevent future issues.
When performed by a trained practitioner, manual cervical decompression has an excellent long-term safety record with rare serious complications. The focus is not just on immediate relief but on preventing symptom recurrence through comprehensive care. This includes patient education on home exercises, posture correction, and lifestyle modifications to support spinal health. High patient satisfaction rates reflect the appreciation for a non-surgical option that provides meaningful, lasting relief.
Risks, Contraindications, and Making an Informed Choice
While manual cervical decompression is safe for most, it is not appropriate for everyone. Understanding the risks and contraindications is essential for making an informed decision.
Potential risks are generally mild and temporary, including muscle soreness or brief dizziness after a session. These typically resolve quickly and can be managed by adjusting the treatment force or duration.
More importantly, there are absolute contraindications where this technique should not be used. These include:
- Spinal instability
- Acute fracture in the cervical spine
- Spinal tumors
- Severe osteoporosis
- Vertebral artery disease
- Acute inflammatory conditions or spinal infections
- Active rheumatoid arthritis affecting the neck
A proper diagnosis is critical to ensure safety. Before treatment, a qualified practitioner will conduct a thorough examination, including a medical history, physical assessment, and review of any imaging (X-rays, MRIs). This determines if manual cervical decompression is a safe and appropriate option for you. Qualified practitioners have extensive training to provide care that is both effective and safe. They are committed to open communication, explaining the rationale, expectations, and any potential risks specific to your condition, empowering you to make confident healthcare choices.
Get your copy of Diving Science Revisited here: https://www.bestpub.com/view-all-products/product/diving-science-revisited/category_pathway-48.html
DISCLAIMER: Articles are for "EDUCATIONAL PURPOSES ONLY", not to be considered advice or recommendations.







