What is Decompression Sickness and How Does It Happen?
What is decompression sickness (DCS) is a medical condition caused by dissolved gases forming bubbles in the blood and tissues due to rapid pressure changes. Also known as "the bends," it most commonly affects scuba divers who ascend too quickly.
Quick Answer:
- Cause: Rapid pressure reduction causes nitrogen bubbles to form in tissues.
- Who's affected: Scuba divers, caisson workers, aviators in unpressurized aircraft.
- Main symptoms: Joint pain, dizziness, numbness, fatigue, confusion.
- Treatment: 100% oxygen and hyperbaric oxygen therapy (recompression).
- Prevention: Slow ascents, safety stops, proper dive planning.
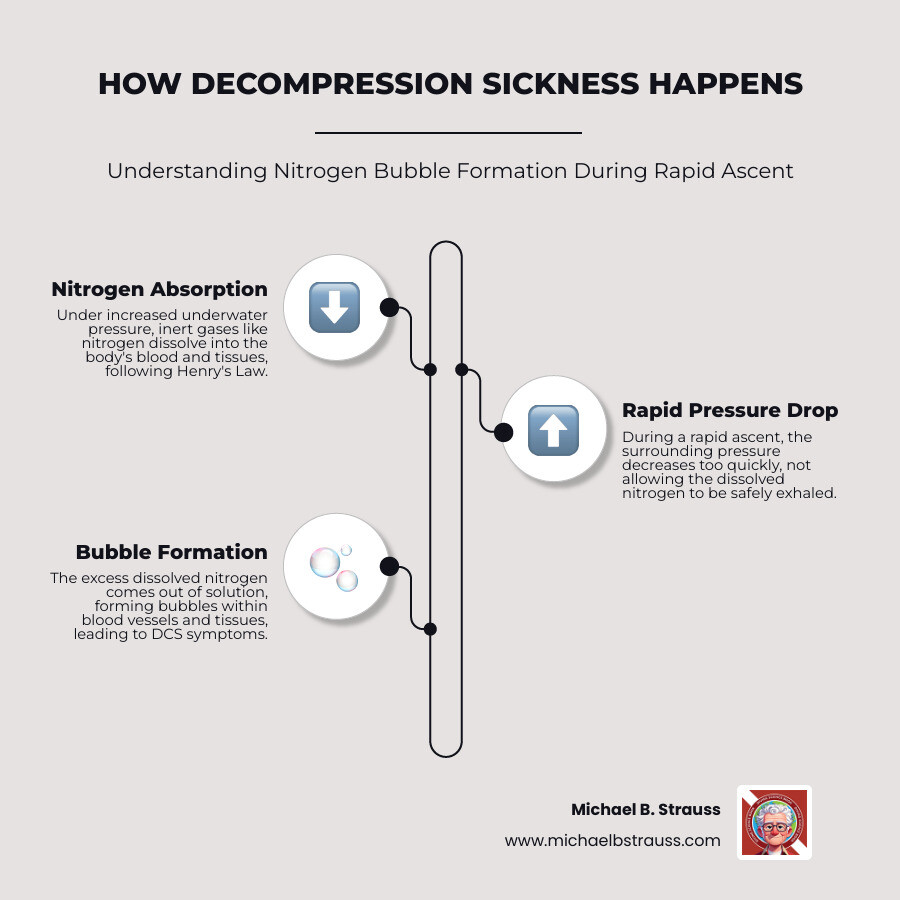
Think of it like opening a carbonated drink too quickly. Underwater, your body absorbs extra nitrogen under pressure. If you ascend too fast, that dissolved nitrogen forms bubbles, similar to how a shaken soda fizzes when opened rapidly. The condition's nickname, "the bends," comes from the severe joint pain that can cause people to bend over in agony.
About 2 to 4 cases occur per 10,000 recreational dives. Crucially, 75% of patients develop symptoms within the first hour after surfacing, though symptoms can appear up to 48 hours later.
What Causes Decompression Sickness?
What causes decompression sickness is explained by Henry's Law: the amount of gas dissolved in a liquid is proportional to the pressure of that gas. When diving, increased ambient pressure forces more nitrogen from the air we breathe to dissolve into our blood and tissues. If the ascent is too quick, the pressure drops rapidly, and the nitrogen comes out of solution to form bubbles before it can be safely exhaled. These bubbles can block blood vessels, damage tissues, and trigger inflammation.
While most common in scuba diving, DCS can occur in any scenario with a rapid pressure drop, including:
- Unpressurized Aircraft Travel: High altitudes expose occupants to lower pressure.
- Caisson Work: Workers exiting pressurized underwater construction environments.
- Space Travel: Astronauts on spacewalks (EVAs).
For a deeper dive into the physics, explore More info about decompression science.
What are the Different Types of DCS?
Decompression sickness is classified by symptom severity to guide treatment.
Type I Decompression Sickness (Less Severe)Type I DCS affects the musculoskeletal system, skin, and lymphatic system. It requires prompt medical attention to prevent progression.
- Pain-Only Bends: The most common sign, characterized by deep, aching pain in or around joints like the shoulders and elbows.
- Skin Bends (Cutaneous DCS): Symptoms include itching and a mottled or marbled rash (cutis marmorata).
Type II Decompression Sickness (More Severe)Type II DCS is more serious, affecting vital organ systems. It is a medical emergency requiring immediate recompression therapy.
- Neurological Symptoms: Bubbles in the brain or spinal cord can cause weakness, paralysis, numbness, tingling, confusion, dizziness (vertigo), and visual or hearing disturbances.
- The Chokes (Pulmonary DCS): A severe form where bubbles obstruct lung capillaries, causing a dry cough, chest pain, and severe difficulty breathing.
- Circulatory Collapse: Widespread bubble formation can lead to shock and organ failure.
Some literature also refers to Type III DCS to describe a severe combination of neurological and pulmonary symptoms.
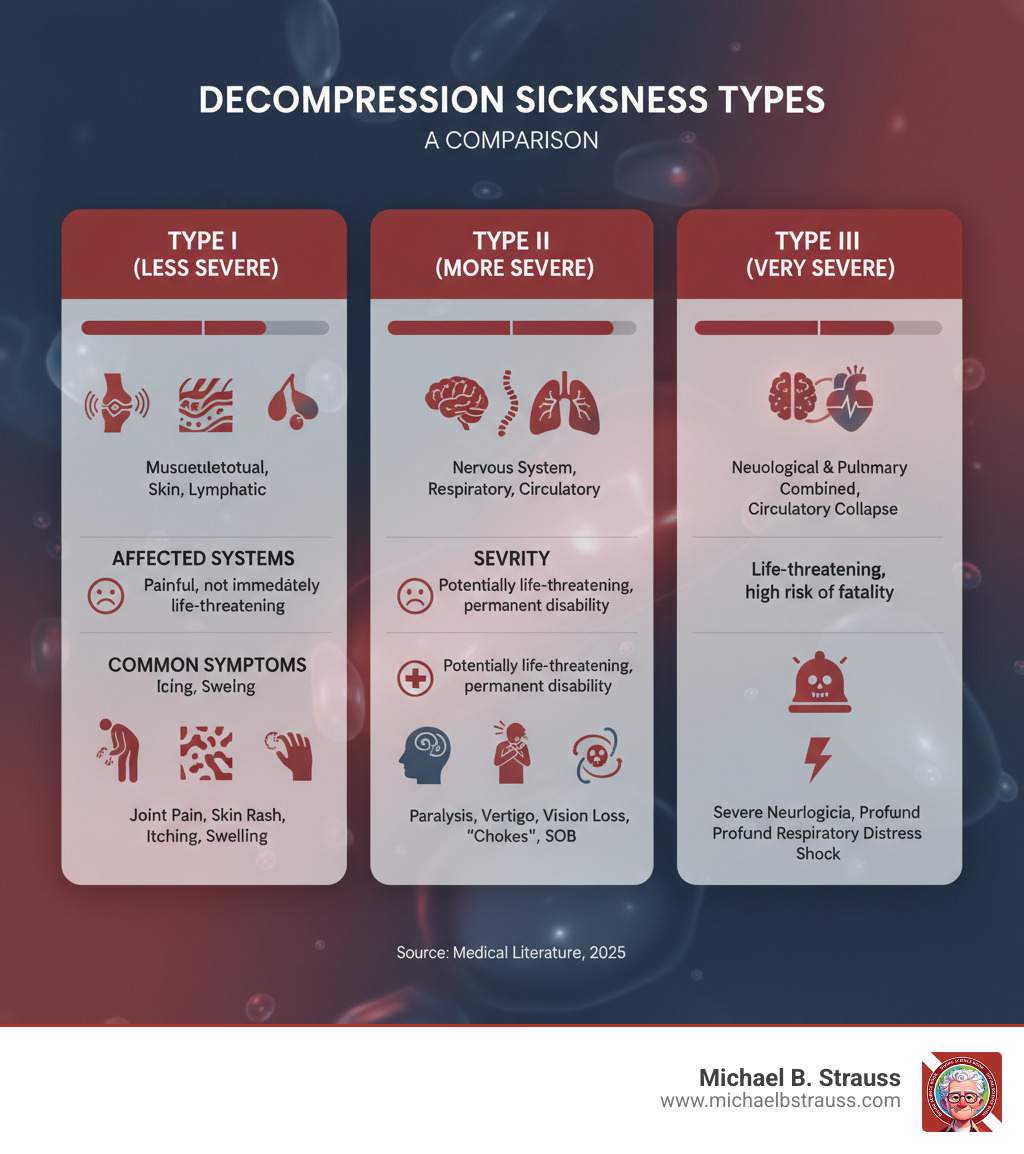
| Feature | Type I DCS (Less Severe) | Type II DCS (More Severe) | Type III DCS (Very Severe) |
|---|---|---|---|
| Affected Systems | Musculoskeletal, Skin, Lymphatic | Nervous System (Brain/Spinal Cord), Respiratory, Circulatory | Neurological & Pulmonary combined, Circulatory Collapse |
| Severity | Painful, but generally not immediately life-threatening | Potentially life-threatening, can cause permanent disability | Life-threatening, high risk of permanent damage or fatality |
| Common Symptoms | Joint pain ("bends"), mottled skin rash (cutis marmorata), itching, mild swelling | Numbness, tingling, paralysis, headache, dizziness, vertigo, confusion, vision/hearing loss, bladder/bowel dysfunction, cough, chest pain ("chokes"), shortness of breath | Severe neurological deficits, profound respiratory distress, shock, unconsciousness |
| Urgency | Urgent medical attention required | Immediate emergency medical attention required | Extreme emergency, critical care needed |
Understanding these types highlights the varied ways DCS can manifest and the importance of timely medical care.
Symptoms, Risks, and Diagnosis
What are the Symptoms of Decompression Sickness?
Recognizing the symptoms of decompression sickness is critical, as they can appear anywhere from immediately after a dive to 48 hours later. While 75% of cases show symptoms within the first hour, this delayed onset can catch divers off guard.
- Joint Pain: The classic sign of "the bends," this is a deep, aching pain, often in the shoulders, elbows, or knees, affecting 60-70% of cases.
- Neurological Symptoms: These are particularly concerning and include numbness, tingling ("pins and needles"), dizziness, vertigo, extreme fatigue, headache, and confusion.
- Severe Symptoms: Paralysis, weakness, shortness of breath, and chest pain ("the chokes") are medical emergencies.
- Skin Manifestations: A mottled, marbled skin rash known as cutis marmorata may appear.

Seek emergency help immediately for any of the following:
- Any neurological symptom (weakness, paralysis, numbness, vision changes, confusion, dizziness)
- Difficulty breathing or chest pain
- Unconsciousness or collapse
- Severe, unrelenting joint pain
- Loss of bladder or bowel control
Even subtle symptoms after a dive warrant caution and medical evaluation.
Who is at Risk for DCS?
While any diver can get decompression sickness, certain factors increase the risk. Understanding these helps you dive smarter.
- Dive Profile: Deep, long, or repetitive dives increase nitrogen absorption. Rapid ascents are a primary controllable risk factor, as they don't allow enough time for nitrogen to be safely exhaled.
- Physiological Factors: Dehydration impairs gas elimination, while obesity increases risk because nitrogen is highly soluble in fat. Increasing age can also reduce circulatory efficiency. A heart condition called a Patent Foramen Ovale (PFO), present in about 25% of people, can significantly increase the risk of serious DCS.
- Environmental and Behavioral Factors: Diving in cold water, heavy exercise during or after a dive, and flying too soon after diving all lift risk. Alcohol consumption contributes to dehydration and should be avoided.
For more on managing diving-related medical concerns, explore more info about diving-related pain.
How is DCS Diagnosed?
Diagnosing decompression sickness is primarily a clinical process, as there is no single definitive test. Doctors act as detectives, combining several pieces of information.
The diagnosis is based on:
- Clinical Evaluation: A thorough assessment of your symptoms, their onset, and progression.
- Dive Profile Review: Your doctor will need to know the depth, duration, and ascent rates of your recent dives, as well as any post-dive altitude exposure.
- Neurological Examination: This is essential for suspected Type II DCS and involves testing motor strength, sensation, balance, and mental status to identify any deficits.
Imaging studies like MRI or CT scans are not used to see bubbles but are valuable for ruling out other conditions with similar symptoms, such as a stroke or spinal cord injury. If DCS is strongly suspected, treatment should begin immediately without waiting for scan results. For the latest on evidence-based care, see scientific research on DCS diagnosis and management.
Treatment, Prevention, and Recovery
How is Decompression Sickness Treated and Prevented?
Effective management of decompression sickness involves both immediate treatment and robust prevention strategies. Knowing how to respond can significantly improve outcomes.
Immediate First AidIf DCS is suspected, act fast. The first steps are:
- Administer 100% Oxygen: Provide the highest possible concentration of oxygen through a tight-fitting mask. This helps flush nitrogen from the body, shrink bubbles, and re-oxygenate tissues.
- Rehydrate: Give the person water to drink if they are conscious and not nauseous. Proper hydration helps restore circulation.
- Position Correctly: Have the person lie flat on their back. If they are unconscious or nauseous, place them in the recovery position on their side.
The Gold Standard: Hyperbaric Oxygen TherapyThe definitive treatment for decompression sickness is Hyperbaric Oxygen Therapy (HBOT). The patient is placed in a hyperbaric chamber where the pressure is increased, physically shrinking the nitrogen bubbles.

While under pressure, the patient breathes pure oxygen. This combination of pressure and high oxygen concentration creates a steep gradient that efficiently removes nitrogen from the body. Treatments follow specific protocols, and while many patients recover after one session, some may require multiple treatments.
Prevention: Your Best DefenseDecompression sickness is almost entirely preventable with safe diving practices.
- Plan Your Dive: Use dive computers or tables to stay within safe limits for depth and time.
- Ascend Slowly: A slow, controlled ascent is non-negotiable. This gives your body time to off-gas dissolved nitrogen naturally.
- Perform Safety Stops: A 3-5 minute stop at around 15 feet (5 meters) provides an extra margin of safety, even on no-decompression dives.
- Wait Before Flying: Follow the no-fly rule. Wait at least 12-24 hours after diving before flying in a commercial aircraft to avoid additional pressure reduction.
- Stay Healthy: Remain well-hydrated and avoid alcohol before and after diving. If you have known risk factors, consult a dive medicine physician.
What is the Prognosis and When Should You Seek Help?
The outlook for decompression sickness is highly dependent on the severity of symptoms and the speed of treatment. With prompt care, the prognosis is generally excellent.
For mild cases (Type I), most people experience a complete resolution of symptoms after HBOT. For more severe cases (Type II), many still make a full recovery, but some may have lingering effects like numbness, chronic pain, or balance issues. The key is immediate action.
The Golden Rule: When in Doubt, Seek HelpSeek help immediately for any suspected symptom of decompression sickness, no matter how minor it seems. Do not wait or hope it will go away. Never attempt to treat DCS by re-entering the water, as this is extremely dangerous.
- Call emergency medical services and state that you are a diver with suspected decompression illness.
- Contact the Divers Alert Network (DAN) for emergencies. DAN's 24-hour hotline provides expert medical guidance and can help locate the nearest hyperbaric chamber.
Dr. Michael B. Strauss's work emphasizes that knowledge and preparation are a diver's best tools. Understanding what is decompression sickness is the first step to ensuring every dive is a safe one.
To deepen your understanding of the science behind diving, get your copy of Diving Science Revisited.
DISCLAIMER: Articles are for "EDUCATIONAL PURPOSES ONLY", not to be considered advice or recommendations.






